What does a Authorization Coordinator do?
An Authorization Coordinator plays a key role in managing the approval process for various transactions and requests. This position ensures that all necessary steps are followed to authorize or decline a request. The coordinator works closely with different departments to gather needed information and documents. They help ensure that each request meets the organization's policies and guidelines.
The duties of an Authorization Coordinator include reviewing requests, verifying information, and communicating with stakeholders. They must have strong attention to detail to ensure accuracy. This role also involves maintaining records of all authorizations and denials. Communication skills are crucial as the coordinator interacts with various teams to facilitate smooth processes. They must be able to handle multiple tasks efficiently and meet deadlines. The coordinator ensures that all authorizations are processed correctly and in a timely manner.
How to become a Authorization Coordinator?
Becoming an Authorization Coordinator offers a rewarding path in the healthcare or insurance industries. This role ensures that medical procedures and services are approved and reimbursed properly. Here is a clear outline to help guide someone through the process.
First, focus on education. A high school diploma or equivalent is the basic requirement. Many employers prefer candidates with an associate's degree in a related field. This education provides a foundation in medical terminology and insurance processes.
- Education: Obtain a high school diploma or GED. An associate's degree in healthcare or insurance is beneficial.
- Experience: Gain experience in a healthcare or insurance setting. Volunteer or work in roles that offer exposure to medical billing or patient services.
- Certification: Pursue certification to enhance qualifications. The National Association of Healthcare Access Management (NAHAM) offers relevant certifications.
- Apply for Positions: Look for job openings as an Authorization Coordinator. Tailor your resume and cover letter to highlight relevant skills and experience.
- Continuous Learning: Stay updated on industry changes. Attend workshops and continue education to improve skills and knowledge.
How long does it take to become a Authorization Coordinator?
Getting the right education is key to becoming an Authorization Coordinator. Most employers prefer candidates with a high school diploma or GED. Some may require further education or training. A certificate or associate degree in medical billing and coding can be very helpful.
The time to get this education varies. A high school diploma takes about four years. A GED can be earned in less time, often within a year. A certificate or degree program can take anywhere from six months to two years, depending on the institution and whether you attend full-time or part-time.
After education, some Authorization Coordinators complete an internship or on-the-job training. This helps them gain practical experience. Training can last a few weeks to several months. With the right education and training, you can start working as an Authorization Coordinator.
Authorization Coordinator Job Description Sample
The Authorization Coordinator is responsible for managing and overseeing the authorization process for various services within the organization. This role involves ensuring compliance with regulatory standards, maintaining relationships with clients and vendors, and streamlining the authorization workflow to improve efficiency.
Responsibilities:
- Manage and coordinate the authorization process for services, ensuring compliance with all regulatory requirements.
- Maintain accurate and up-to-date records of authorizations, ensuring all documentation is complete and properly filed.
- Collaborate with clients and vendors to ensure all necessary information is provided for the authorization process.
- Conduct regular audits of the authorization process to identify areas for improvement and implement changes as needed.
- Communicate with internal departments to resolve any authorization-related issues and provide guidance on authorization procedures.
Qualifications
- Bachelor’s degree in Business Administration, Healthcare Management, or a related field.
- Minimum of 3 years of experience in an authorization or related role.
- Strong understanding of regulatory requirements and industry standards.
- Excellent communication and interpersonal skills.
- Ability to manage multiple tasks and prioritize workload effectively.
Is becoming a Authorization Coordinator a good career path?
An Authorization Coordinator plays a crucial role in the healthcare industry. They work with insurance companies to ensure patients receive necessary medical care. This role involves reviewing patient information and verifying insurance details. It is a job that requires attention to detail and strong communication skills.
Choosing this career path has its own set of advantages and disadvantages. On the positive side, it offers a stable job with good earning potential. It also provides opportunities to work closely with patients and healthcare professionals. However, the job can be stressful due to the need to meet tight deadlines and handle sensitive information. It may also require working outside of regular office hours.
Consider these pros and cons before pursuing this career:
- Pros:
- Stable job with good earning potential
- Opportunities to work with patients and healthcare professionals
- Skills development in communication and organization
- Cons:
- High stress levels due to deadlines
- Handling sensitive patient information
- Potential for irregular working hours
What is the job outlook for a Authorization Coordinator?
Job seekers interested in becoming an Authorization Coordinator will find a stable employment landscape. The Bureau of Labor Statistics (BLS) reports an average of 600 job positions available each year. Despite a projected decrease of 5.9% in job openings from 2022 to 2032, this role remains a viable career path. Those entering this field should focus on developing strong skills and qualifications to stand out in the job market.
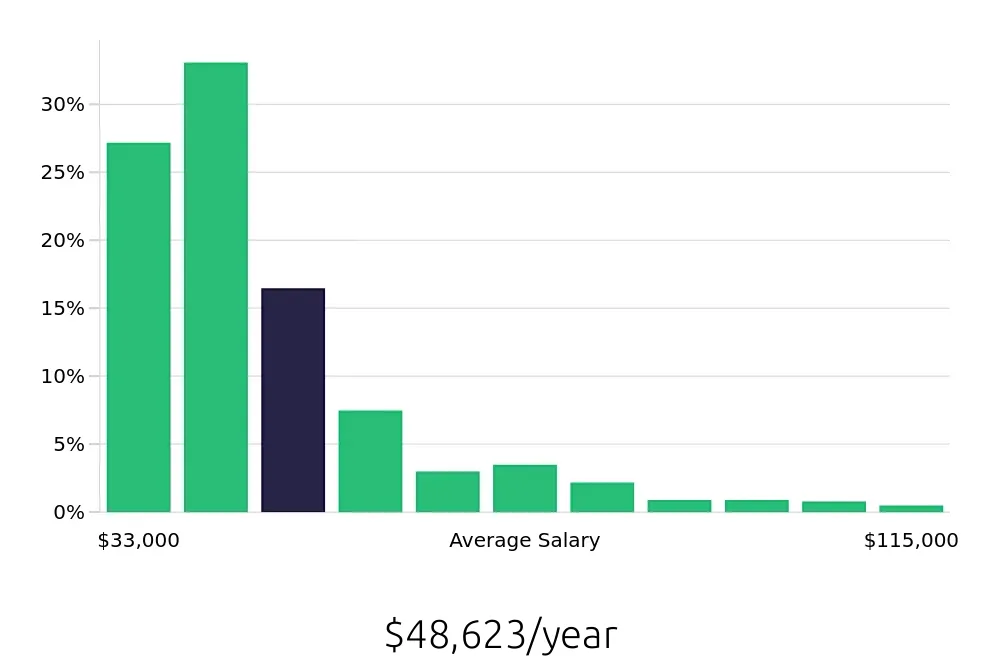
Authorization Coordinators enjoy a competitive salary. The BLS reports an average national annual compensation of $46,940. This means individuals in this role can expect a steady income. Additionally, the average hourly compensation stands at $22.57, providing a clear view of the earning potential. This financial outlook can be appealing for many job seekers considering this career.
In summary, the Authorization Coordinator role offers a balanced mix of job security and financial rewards. With approximately 600 job positions opening annually, and a solid average salary, this career remains attractive. Job seekers should leverage this information to make informed decisions about their professional future. Staying updated on trends and skills in this field will enhance their prospects. For more detailed data, visit the BLS website.
Currently 124 Authorization Coordinator job openings, nationwide.
Continue to Salaries for Authorization Coordinator