What does a Utilization Review Coordinator do?
A Utilization Review Coordinator plays a key role in the healthcare industry. This professional ensures that patients receive the right care at the right time. They review medical records and treatments to make sure everything aligns with insurance guidelines. This helps avoid unnecessary costs and ensures patients get the best care possible.
The coordinator works closely with doctors, nurses, and insurance companies. They communicate about the patient's care plan and insurance coverage. They check if treatments are medically necessary and approved by insurance. This helps keep healthcare costs under control and improves patient outcomes. The coordinator must be detail-oriented and well-organized to handle these tasks effectively.
The job requires strong communication skills. The coordinator needs to explain insurance details to patients and staff. They also need to write clear reports. This position demands knowledge of medical procedures and insurance policies. It is a vital role that supports both the healthcare providers and the patients.
How to become a Utilization Review Coordinator?
Becoming a Utilization Review Coordinator is a rewarding career choice that requires certain steps. This role involves reviewing patient care to ensure that it meets quality and cost-effectiveness standards. By following a structured process, one can navigate through educational and professional requirements successfully.
To embark on this career, consider these steps:
- Complete high school or obtain a GED.
- Earn an associate or bachelor’s degree in health administration, healthcare management, or a related field.
- Gain experience in a healthcare setting through internships or entry-level jobs.
- Obtain necessary certifications, such as the Certified Utilization Review Practitioner (CURP) credential.
- Apply for positions as a Utilization Review Coordinator and continue professional development.
How long does it take to become a Utilization Review Coordinator?
The journey to becoming a Utilization Review Coordinator offers a clear and rewarding path for those interested in healthcare management. Generally, it takes about 2-4 years to gain the necessary qualifications. Most start with a high school diploma or equivalent. Then, they pursue a post-secondary certificate or associate's degree in health information management or a related field. These programs cover important topics like medical coding, billing, and healthcare law.
After completing their education, aspiring coordinators often gain practical experience. Many start with entry-level jobs in medical records or billing. This hands-on work helps them understand the healthcare system and builds the skills needed for utilization review. Some coordinators may choose to pursue certification, which can enhance job prospects and offer more opportunities for advancement. Overall, dedication and continued learning can lead to a stable and fulfilling career in healthcare management.
Utilization Review Coordinator Job Description Sample
A Utilization Review Coordinator is responsible for evaluating the necessity and efficiency of healthcare services provided to patients. This role involves reviewing patient care to ensure that it meets established medical criteria and to promote cost-effective healthcare delivery.
Responsibilities:
- Conduct comprehensive reviews of patient care to ensure medical necessity and appropriateness of services.
- Collaborate with healthcare providers to develop care plans and coordinate patient care.
- Utilize clinical criteria and guidelines to evaluate patient care and make informed decisions.
- Communicate with insurance companies to ensure compliance with coverage policies and requirements.
- Maintain accurate and detailed documentation of all review activities and outcomes.
Qualifications
- Bachelor's degree in Healthcare Administration, Nursing, or a related field.
- Certification in Utilization Review (e.g., CURN, CURS) preferred.
- Minimum of 2-3 years of experience in a healthcare setting, preferably in utilization review or case management.
- Strong understanding of medical terminology, healthcare policies, and insurance processes.
- Excellent analytical and critical thinking skills with the ability to interpret clinical data.
Is becoming a Utilization Review Coordinator a good career path?
A Utilization Review Coordinator checks if patients get the care they need. They work in hospitals and insurance companies. This role involves reviewing medical records to ensure treatments and services are necessary. It plays a key part in managing healthcare costs and improving patient care.
Being a Utilization Review Coordinator has many benefits and some challenges. Let's look at both.
- Pros:
- Job Stability: Many hospitals and healthcare facilities need these coordinators.
- Competitive Pay: This role often comes with a good salary and benefits.
- Variety of Work: Tasks can range from reviewing records to speaking with healthcare providers.
- Helping Others: Coordinators ensure patients get the right care, which can be very rewarding.
- Cons:
- Stressful Situations: Dealing with medical issues and insurance claims can be tough.
- Long Hours: The job can require working beyond regular hours, especially during busy times.
- Detail-Oriented: Must be very careful to avoid mistakes in medical records and billing.
- Constant Learning: New laws and healthcare policies mean ongoing education is necessary.
What is the job outlook for a Utilization Review Coordinator?
The job outlook for Utilization Review Coordinators remains strong, with an average of 7,200 positions opening each year, as reported by the Bureau of Labor Statistics (BLS). This consistent demand indicates a reliable career path for those seeking employment in this field. The BLS also projects an 8.5% growth in job openings from 2022 to 2032. This growth suggests that more opportunities will become available in the coming years, making it an attractive field for job seekers.
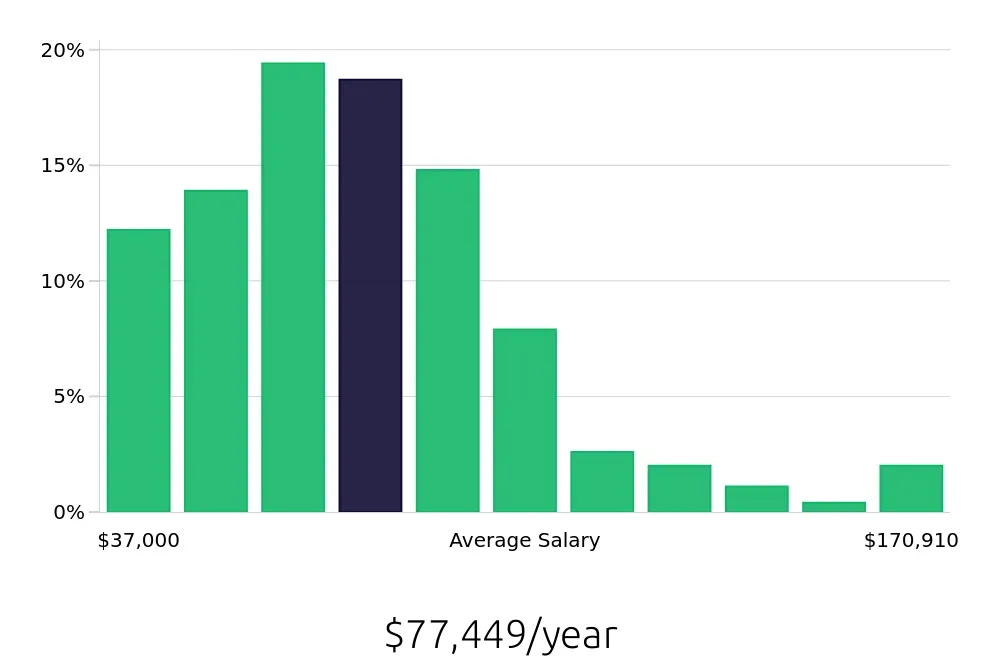
The average national annual compensation for Utilization Review Coordinators stands at $67,520, according to the BLS. This figure reflects the value of the skills and responsibilities associated with the role. Additionally, the average hourly wage is $32.46. These figures underscore the potential for a rewarding financial career in this profession. As healthcare needs continue to evolve, the role of a Utilization Review Coordinator becomes increasingly vital, potentially leading to higher demand and compensation.
Apart from the financial benefits, a career as a Utilization Review Coordinator offers stability and growth potential. This role plays a crucial part in the healthcare industry, ensuring that patients receive appropriate care. For job seekers, this translates to not only a promising job outlook but also the chance to make a meaningful impact in patient care. With consistent job openings and positive growth projections, this career path presents a promising opportunity for those looking to enter the healthcare sector.
Currently 134 Utilization Review Coordinator job openings, nationwide.
Continue to Salaries for Utilization Review Coordinator