How much does a Utilization Review Coordinator make?
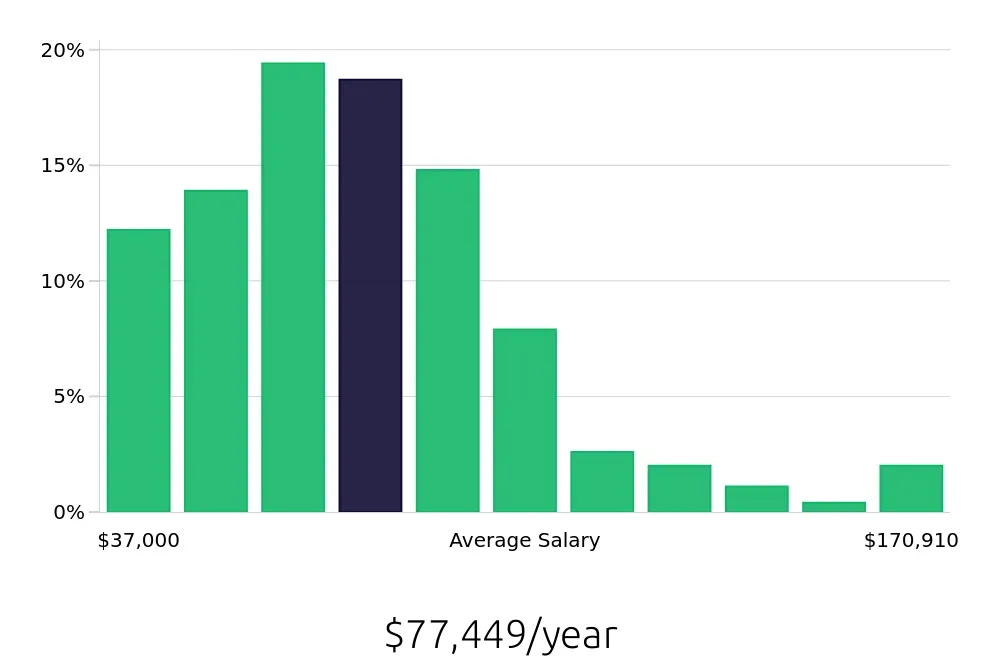
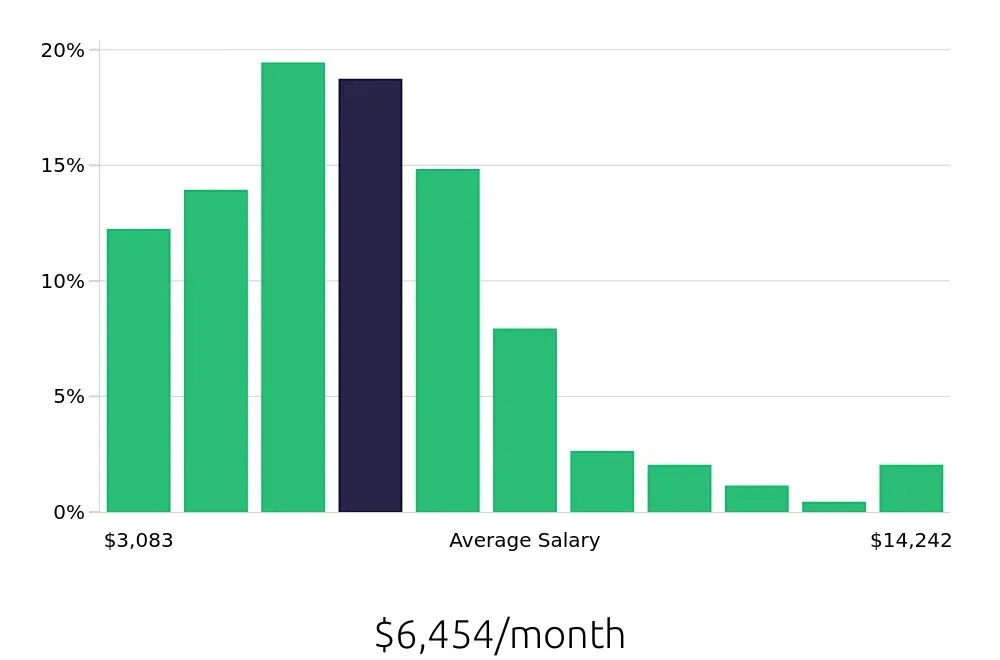
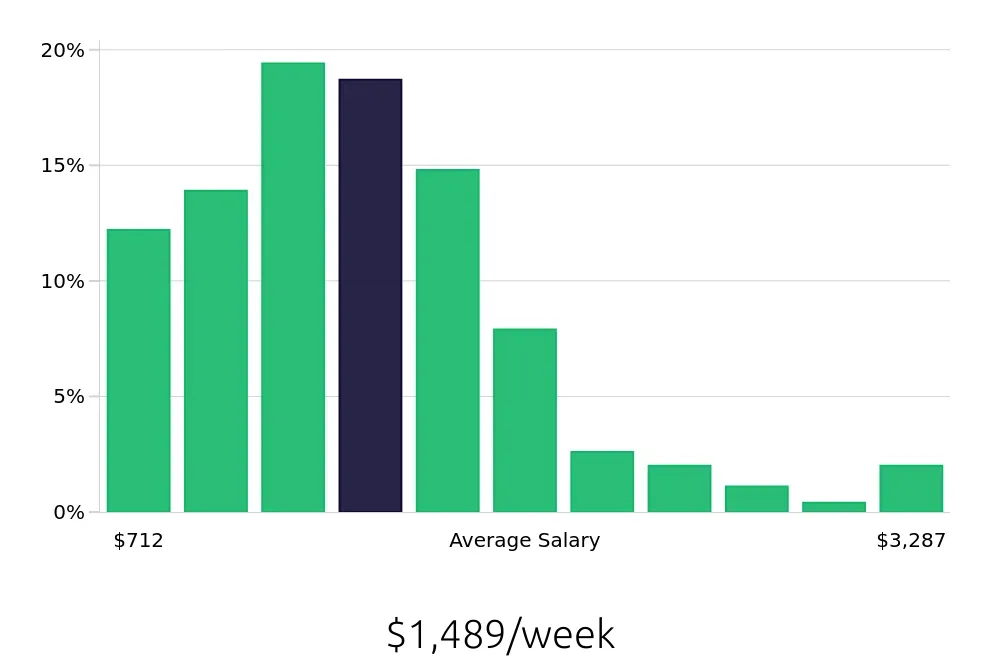
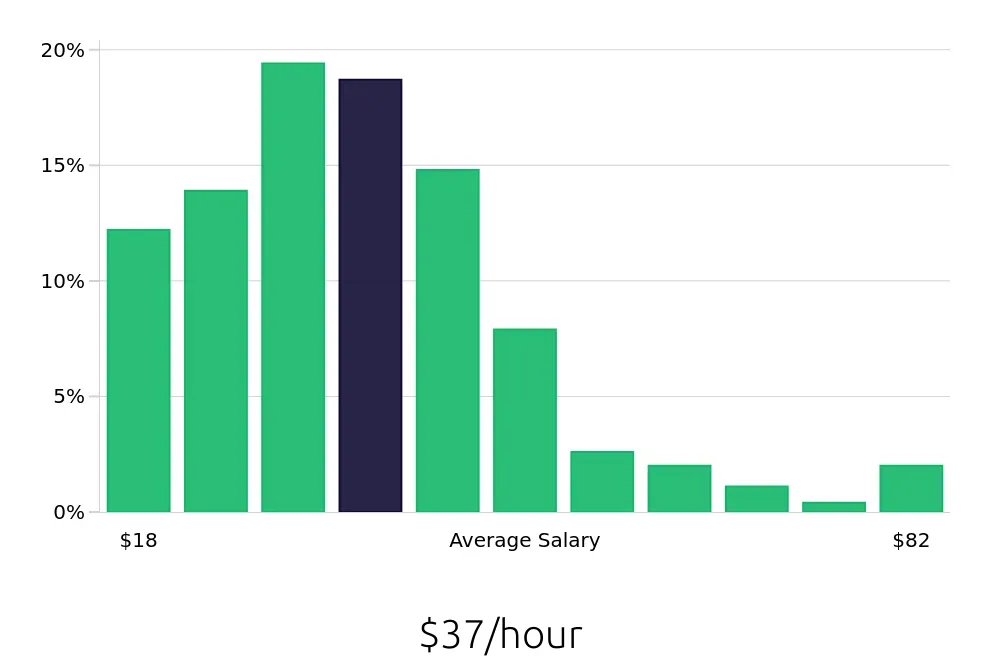
A Utilization Review Coordinator plays a key role in healthcare. This person works to ensure that patients get the care they need. They check if the care being provided is necessary and fits the guidelines set by insurance companies. The average yearly salary for this job is $77,449. This average helps people understand what to expect in terms of earnings.
The salary for a Utilization Review Coordinator can vary based on experience and location. Most coordinators earn between $37,000 and $170,910 annually. This range shows that with more experience, the salary can increase. Some key factors affecting salary include the size of the hospital, the specific duties of the role, and the region where the coordinator works.
What are the highest paying cities for a Utilization Review Coordinator?

-
Fresno, CA
Average Salary: $103,712
In Fresno, individuals in this role assist healthcare facilities in managing patient care efficiency. They work with prominent companies such as Kaiser Permanente and Community Regional Medical Center. Professionals here ensure care aligns with medical necessity and cost-effectiveness.
Find Utilization Review Coordinator jobs in Fresno, CA
-
Washington, DC
Average Salary: $100,243
In the capital, professionals in this field play a key role in optimizing healthcare services. They often collaborate with healthcare giants like MedStar Health and Johns Hopkins Medicine. Their work helps ensure patients receive appropriate care and facilities run smoothly.
Find Utilization Review Coordinator jobs in Washington, DC
-
San Diego, CA
Average Salary: $95,599
In San Diego, these coordinators support high-quality care delivery. They work with top employers like Scripps Health and Sharp HealthCare. They analyze treatment plans and patient needs to support effective healthcare services.
Find Utilization Review Coordinator jobs in San Diego, CA
-
San Jose, CA
Average Salary: $93,963
In San Jose, coordinators assist in managing patient care efficiently. They often work with companies like Stanford Health Care and Kaiser Permanente. They ensure medical procedures are both necessary and cost-effective.
Find Utilization Review Coordinator jobs in San Jose, CA
-
Atlanta, GA
Average Salary: $90,725
Atlanta offers opportunities in this field with major healthcare providers like Emory Healthcare and Northside Hospital. Coordinators here focus on improving patient care and reducing unnecessary treatments, ensuring quality and efficiency.
Find Utilization Review Coordinator jobs in Atlanta, GA
-
Chicago, IL
Average Salary: $85,120
In Chicago, professionals can find roles with healthcare leaders such as Northwestern Memorial Hospital and Rush University Medical Center. They review care plans to support effective and necessary treatments for patients.
Find Utilization Review Coordinator jobs in Chicago, IL
-
Buffalo, NY
Average Salary: $84,849
Buffalo provides a range of opportunities with employers like Kaleida Health and ECMC. These professionals ensure that patient care aligns with medical guidelines and financial constraints.
Find Utilization Review Coordinator jobs in Buffalo, NY
-
Riverside, CA
Average Salary: $83,001
In Riverside, coordinators assist in ensuring patient care meets medical standards. They work with institutions such as Riverside University Health System. Their efforts contribute to efficient and effective healthcare services.
Find Utilization Review Coordinator jobs in Riverside, CA
-
Los Angeles, CA
Average Salary: $82,837
Los Angeles offers many positions with healthcare giants like Cedars-Sinai Medical Center and UCLA Health. Coordinators here focus on improving patient care while keeping costs manageable.
Find Utilization Review Coordinator jobs in Los Angeles, CA
-
Houston, TX
Average Salary: $81,189
In Houston, professionals work with major healthcare providers such as Houston Methodist and Baylor St. Luke’s Medical Center. They ensure care plans meet both patient needs and financial guidelines.
Find Utilization Review Coordinator jobs in Houston, TX
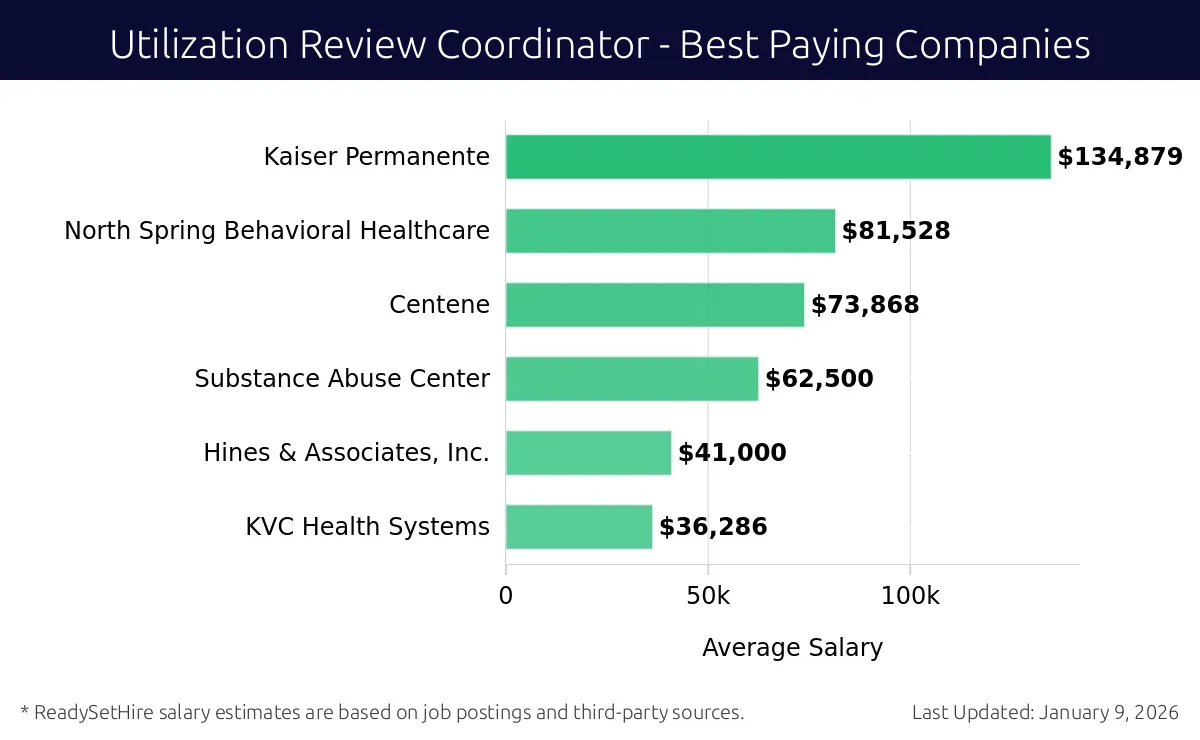
What are the best companies a Utilization Review Coordinator can work for?
-
Kaiser Permanente
Average Salary: $134,879
Kaiser Permanente offers competitive salaries for Utilization Review Coordinators. They operate nationwide, with major locations in California, Colorado, Georgia, Maryland, and Virginia. Kaiser focuses on providing comprehensive healthcare services, and their coordinators play a key role in managing patient care and insurance benefits.
-
North Spring Behavioral Healthcare
Average Salary: $81,528
North Spring Behavioral Healthcare provides a good salary for Utilization Review Coordinators. They serve locations across Virginia and Ohio. This company is dedicated to mental health and substance abuse treatment, offering a supportive environment for their staff to excel.
-
Centene
Average Salary: $73,868
Centene offers a solid salary for Utilization Review Coordinators. They operate in multiple states, including Florida, Missouri, and Ohio. Centene is a leading health services company focusing on government-sponsored programs, providing valuable opportunities for professionals in this field.
-
Substance Abuse Center
Average Salary: $62,500
The Substance Abuse Center pays around $62,500 for Utilization Review Coordinators. They have locations in various states, including California and Washington. This center is committed to helping individuals struggling with addiction, creating a meaningful work environment for coordinators.
-
Hines & Associates, Inc.
Average Salary: $41,000
Hines & Associates, Inc. provides a decent salary for Utilization Review Coordinators. They are based in South Carolina. This company offers specialized services in healthcare and insurance, providing an opportunity for coordinators to make a significant impact.
-
KVC Health Systems
Average Salary: $36,286
KVC Health Systems offers a lower salary of around $36,286 for Utilization Review Coordinators. They operate in Kansas, Missouri, and Utah. This nonprofit organization focuses on children and family services, offering a supportive and community-driven work environment.
How to earn more as a Utilization Review Coordinator?
A Utilization Review Coordinator has the opportunity to enhance earnings through various professional strategies. Each tactic presents a pathway to increase not only skills but also market value in the healthcare industry. Building expertise and seeking growth can lead to higher salary potential and career advancement.
Key factors include gaining relevant certifications, expanding job experience, pursuing higher education, developing strong communication skills, and staying updated on industry trends. Each of these elements can significantly impact earnings and career progression.
Here are five factors to consider:
- Certifications: Earning professional certifications can boost credibility and open new career paths. For example, the Certified Utilization Review Practitioner (CURP) credential demonstrates specialized knowledge.
- Experience: Gaining experience in various healthcare settings can make a candidate more versatile and valuable. More experience often translates to higher earning potential.
- Education: Higher education, such as a bachelor's or master's degree in healthcare administration, can lead to better job opportunities and higher salaries.
- Communication Skills: Strong communication skills are vital. They help in effectively interacting with healthcare providers and patients, leading to better job performance and promotions.
- Industry Knowledge: Staying informed about healthcare laws, policies, and trends ensures a coordinator remains competitive. This knowledge can lead to better decision-making and increased job effectiveness.